Biomedical engineering undergrads design and produce medical training simulators for doctoral students in the Nurse Anesthesia program.
This collaboration is important because it bridges the gap between engineering and healthcare, fostering interdisciplinary learning and innovation.
— Susan Freudzon, PhD, Professor of the Practice of Biomedical Engineering
On the second floor of the Marion Peckham Egan School of Nursing and Health Studies, nurse anesthesia residents are clustered around a procedure table set up with ultrasound equipment and five lifelike silicone neck and shoulder models. With steady hands, they practice inserting needles into the model necks and guiding ultrasound wands across the skin like surfaces, their eyes focused on screens as live images of the needles, nerves, and structures within the necks come into view.
This is not just any training exercise; it is an ultrasound-guided regional anesthesia simulation for a peripheral nerve block. The silicone neck models, complete with 3D-printed collarbones and plastic tubing that mimics nerve threads, offer students in the Doctor of Nursing Practice (DNP) in Nurse Anesthesia program hands-on practice in administering a peripheral block near nerve regions — a necessary technique they will someday use on real patients in healthcare settings.
The models used during the simulation are the result of an innovative collaboration between Fairfield Egan and the School of Engineering and Computing, driven by a surge in enrollment in the DNP-Nurse Anesthesia program, which has recently expanded to Fairfield’s Austin, Texas campus.
The influx of new nurse anesthesia students highlighted a critical need for additional simulation training resources. Tasked with the design of low-cost, high quality training tools for the DNP students, undergraduates in Fairfield’s Biomedical Engineering program rose to the challenge.
“This collaboration is important because it bridges the gap between engineering and healthcare, fostering interdisciplinary learning and innovation,” said Susan Freudzon, PhD, professor of the practice of biomedical engineering.
Two engineering design projects — the custom silicone neck and shoulder models described above, and a previous trachea model (see sidebar) — were the results of multiple collaborative meetings, test runs, and refinements over the course of a year. Working together on these models enhanced the nurse anesthesia residents’ understanding of the technical aspects of the medical devices they use, and also improved their practical skills. For the biomedical engineering students, engaging with clinical applications and facing real-world healthcare challenges ensured their designs were both practical and effective.
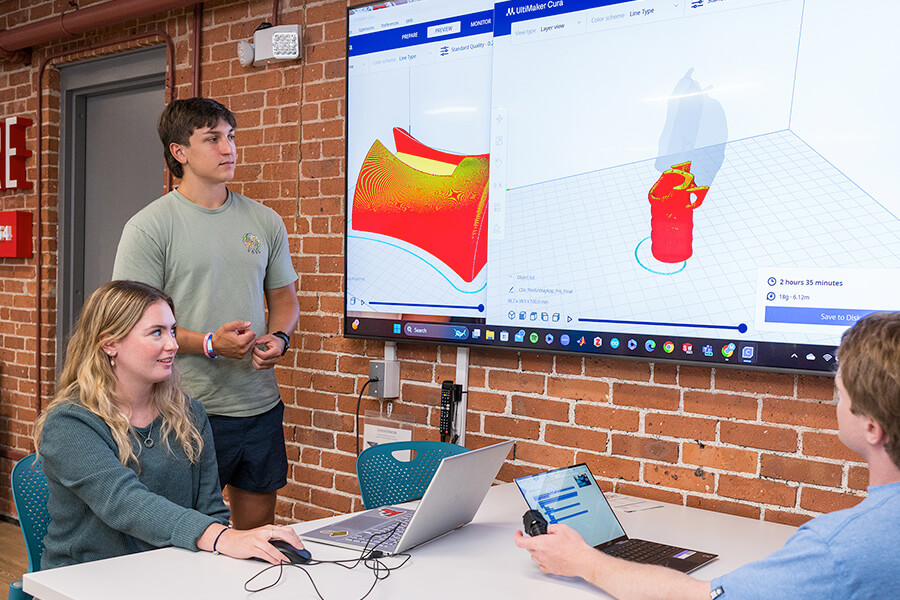
Engineering students Maeve O’Connell ’25 and Matthew Manduca ’25 assess a trachea neck design in the Innovation Annex.
“From a faculty perspective, it was rewarding to see the students’ learning evolve as they went through the design process,” said Dr. Freudzon.
Custom-built in the School of Engineering and Computing’s Innovation Annex, the silicone necks were designed as a senior capstone project by Emma Crowley ’24, Julia Kilroy ’24, Ryan Baker ’24, and Wilson Kaznoski ’24. They are known as ultrasound phantom models and take roughly 12 hours each to make. Ultrasound phantoms are essential tools for simulation, providing a “stand-in” for real human tissue that can be scanned or imaged. The bioengineering team’s reusable, low-cost phantom devices have proven to be indispensable models for nurse anesthesia students to practice their skills on.
“The silicone neck aids us in performing upper extremity regional blocks and allows us to practice our ultrasound skills while also attempting to provide us with realistic human anatomy,” said Steven Santiago, a nurse anesthesia student in the DNP program. “The collaboration between our two programs not only helps hone our clinical skills, but also allows us to help the engineering students by providing feedback on their project.”
A big challenge for the biomedical engineering students came when choosing the right type of silicone to best imitate human skin. If the silicone is too stiff, the nurse anesthesia residents are not able to maneuver the needle. If the silicone is too soft, the material will crack from repeated use, resulting in puncture pathways that inhibit the residents’ ability to locate nerves independently. Additionally, the type of silicone used impacts how the needle and neck structures appear on the ultrasound.
Through a trial-and-error design process, the biomedical engineers overcame obstacles such as the silicone not curing properly and the 3D-printed nerve network and collarbone appearing fuzzy on the ultrasound.
“I’m a biomedical engineering major, but I’m also a pre-physician’s assistant,” noted Emma Crowley, “so being able to meet with the nursing students and professors to learn how the procedure is done and to get feedback was helpful.”
Reflecting on the many tweaks and improvements made during the design phase, she noted, “My anatomy class also helped me understand how to improve the design of the mold and what it needed to look like on the ultrasound.”
The seniors presented their capstone project, titled “Ultrasound Phantom for Regional Anesthesia,” and won first place in the student poster session of the 2024 ASEE (American Society of Electrical Engineers) Northeast Conference, which drew a record breaking attendance and was hosted by Fairfield University in April.

Dr. Susan Freudzon and Ryan Jaworski ’25 review a newly 3D-printed trachea prototype.
Simulation coordinator and assistant professor of the practice Christine Aloi, DNP, CRNA, APRN, noted that the partnership with the Biomedical Engineering program “has greatly benefited the Nurse Anesthesia program. Our cohort has grown, and the engineering team has supplied us with several silicone neck models for use in a single lab setting. This enables multiple nurse anesthesia residents to practice this skill simultaneously, providing them more time and experience in the simulated placement of this particular peripheral nerve block of the upper extremity under ultrasound guidance.”
The two schools plan to continue their collaboration next year. Based on feedback received this summer, Dr. Freudzon’s biomedical engineering students will further modify designs to create a series of models with varying skin thicknesses that better simulate the range found among patients. There is also a plan to supply models to the newly launched DNP-Nurse Anesthesia program in Austin, Texas.
“This collaboration is the beginning of a wonderful partnership between biomedical engineering students and nurse anesthesia students,” said Dr. Freudzon. “We have already discussed future projects and plan to innovate and work together to continue to produce educational training tools that can be used to enhance clinical training and improve patient care.”
An Affordable, Anatomically Correct Trachea Model
The first collaboration between Fairfield’s biomedical engineering students and nurse anesthesia residents resulted in the design and 3D-printing of a low-cost, anatomically correct trachea model, which allows the DNP students to practice airway management skills and cricothyrotomy — an emergency surgical intervention for creating an airway when traditional intubation is not possible.
In response to feedback from the Fairfield Egan students, biomedical engineering undergrads Emma Crowley ’24, Ryan Jaworski ’25, Matthew Manduca ’25, and Maeve O’Connell ’25 developed a unique trachea model that features a 3D-printed neck-shaped base to stabilize the trachea, and artificial skin using “tattoo skin” — which has lifelike texture and response, and is used for practice by tattoo artists. The trachea model takes about two and a half hours to print on the 3D printers in the School of Engineering and Computing’s Innovation Annex.








